Last Updates
The Australian Government has rolled out the new Aged Care Act 2024 since November 1, 2025.
Therefore, we recommend you check this blog frequently for any future updates. Last Updated on 6/11/2025.
The most recent amendments are listed below:
- New Registration Application forms are formally released.
- New Quarterly Budget for the 8 classifications of support-at-home services
- Fees for provider applications transitioned to the new Act
Brief History of Aged Care Reforms and Why They Are Needed
The Royal Commission into Aged Care Quality and Safety was established in 2018 in response to systemic gaps identified in the aged care system, resulting in the neglect of older people and barriers to accessing quality aged care services for all who need them.
In response to the findings released in 2021, many reforms were implemented immediately, and others have been rolled out since then.
The changes that have been implemented represent the most significant improvements from the Royal Commission and put the rights of older people at the centre of care and services, holding providers to account.
New Terminology
| Term | Definition | Previously Known As |
|---|---|---|
| Aged Care Worker | Employees, contractors, and volunteers of an aged care provider | Worker, staff |
| AT-HM Scheme | Funding is available for Support at Home participants for Assistive Technology and Home Modifications. | GEAT, Goods, Equipment, Assistive Technology, Home Modifications. |
| Care Partner | A person who provides care management for participants in an ongoing class (1-8) or who is accessing the End-of-Life Pathway | Case Manager, Care Coordinator |
| Restorative Care Partner | A person with relevant university health-related qualifications who provides care management services for participants accessing the Restorative Care Pathway. | Case Manager, Care Coordinator |
| Continuity of Care | The Aged Care Act definition has not yet been released. | Security of tenure |
| End-of-Life Pathway | A short-term funding stream is available under Support at Home for participants who have been diagnosed with a life expectancy of 3 months or less and wish to remain at home. | Not previously provided under the Home Care Package Program |
| Funded aged care services | Aged care services are delivered by registered providers who receive government subsidies. | Care and services |
| Individual | A person eligible for or receiving funded aged care services | Older person, consumer, |
| Integrated Assessment Tool (IAT) | The new assessment tool is used to determine an older person’s eligibility for aged care services. | National Screening Assessment Form (NSAF) |
| Participant | An individual received funded aged care services through the Support at Home Program | Home care package recipient, consumer, client |
| Registered provider | A provider of funded aged care services who has been approved and registered by the Aged Care Quality Commission. | Approved provider |
| Responsible Person | Any person who:
|
Key Personnel |
| Restorative Care Pathway | A short-term pathway providing up to 12 weeks of intensive allied health and/or nursing services and supports aimed at helping the participant regain function and/or manage new or changing age-related conditions. | Short-term Restorative Care, Flexible Care |
| Rules | The Aged Care Act is subordinate legislation. | Principles (Quality of Care, User Rights, Accountability, etc.) |
| Statement of Rights | The rights to which individuals are entitled are set out in Section 23 of the Aged Care Act 2024. | Charter of Aged Care Rights, the Charter |
| Strengthened Aged Care Quality Standards | The new Aged Care Quality Standards have been effective from 1 November 2025. | Aged Care Quality Standards |
| Supporter | A person or persons nominated by an individual to assist them in their decision-making. Supporters are registered with My Aged Care. | Representative, next of kin |
| Associated Provider | Any other organisation or individual person engaged to deliver funded aged care services on behalf of the registered provider. | Subcontractor or external provider. |
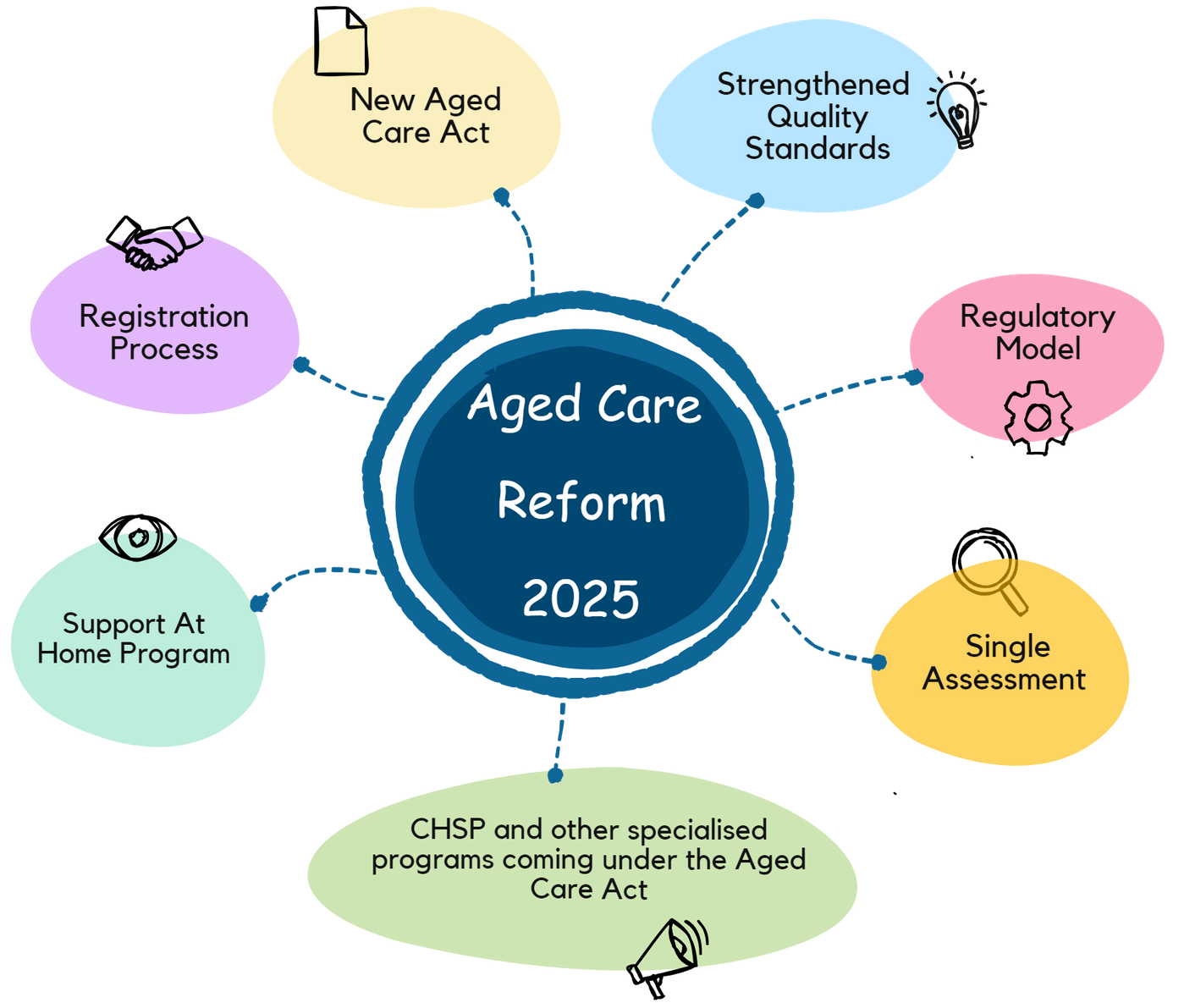
Key Features of the Changes on 1 November 2025
New Aged Care Act and Rules
The Aged Care Bill 2024 was passed through parliament towards the end of 2024, and since then, further consultation has been undertaken to finalise the subordinate legislation, which is known as the Rules (previously referred to as the Principles).
The new Aged Care Act 2024 contains a number of improvements on the previous Act, including:
- strengthens the rights of people accessing aged care services
- introduces enhanced system requirements for information management and complaints management
- streamlines, clarifies, and enforces the provider obligations
- introduces a new registration process and regulatory model
- introduces new supported decision-making processes
- stronger whistleblower protections for individuals, workers, and others who report breaches of Aged Care laws.
More information on the new Aged Care Act can be found here: https://www.health.gov.au/our-work/aged-care-act
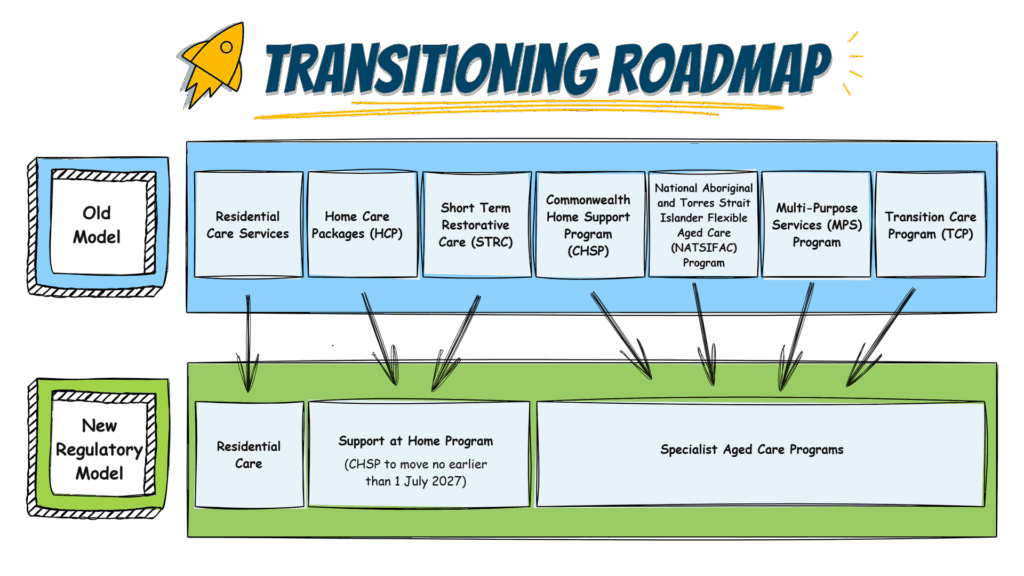
Old Aged Care Programs and the New Regulatory Model
The infographic below illustrates how aged care programs will be transitioned to the new regulatory model, noting that the Commonwealth Home Support Program will only be fully integrated under the Support at Home Program in 2027 and cease to exist as a standalone program. Until then, it will be referred to as the Specialist Aged Care Program but will be regulated under the new Aged Care Act (see CHSP Providers section for more details)
The other aged care programs depicted in the diagram below, which are known as Specialist Aged Care Programs from 1 November 2025, are:
- The National Aboriginal and Torres Strait Islander Flexible Aged Care (NATSIFAC) Program provides funding to providers for the delivery of culturally safe and flexible care to older Aboriginal and Torres Strait Islander people in a way that keeps them connected to their home and community and can include residential and home care services. NATSIFAC is not be merged with the Support at Home Program and continues to operate outside of the Aged Care Act.
- The Multipurpose Services (MPS) Program is designed to deliver health and aged care services in rural and remote communities whose populations are too small to support both a hospital and a residential aged care home. It is not be merged with the Support at Home Program as MPS providers deliver residential care; however, it changes in line with other reforms under the new Aged Care Act.
- The Transition Care Program (TCP) is a flexible care program that delivers therapy-focused services to assist older people in recovering after a hospital stay of up to 12 weeks. It is regulated under the Aged Care Act; however, there are no plans to integrate this program with the incoming Support at Home Program; therefore, it continues to operate as a Specialist Aged Care Program.
Provider Obligations and Responsibilities
Many existing provider obligations and responsibilities remain in place or be amended or strengthened.
In summary, though, ALL registered aged care providers are required to continue meeting the following obligations:
- Meet the Strengthened Aged Care Quality Standards
- Retain an adequate number of skilled staff
- Continuous improvement
- Ensure the suitability of the Responsible Persons
- Ensure all aged care workers have clearances
- Only charge certain fees and prices
- Service agreements for individuals receiving residential care or support at home
- Legislated reporting, such as Aged Care Financial Reporting, Quarterly Reports, Serious Incidents, and Material Changes.
- Provider governance arrangements
- Cooperate with the Aged Care Quality and Safety Commission
- Keeping records
- Deliver care and services consistent with the Statement of Rights
- Meet the Code of Conduct for Aged Care
- Protect personal information
- Complaints resolution and whistleblower policy
- Manage and prevent incidents
- Provide continuity of care
- Access by supporters and independent aged care advocates
The Aged Care Quality and Safety Commission has released a Provider Governance Policy that came into effect on 1 November 2025. The policy provides guidance for registered providers on the role of good governance in delivering safe, high-quality care to individuals, ensuring compliance with a provider’s responsibilities and obligations, and supporting the success and sustainability of an organisation. The policy outlines the following key aspects of provider governance:
- The Commission’s expectations of registered providers
- The guiding principles for good provider governance
- Provider governance obligations
- How the Commission collects provider governance information
- How the Commission responds to provider governance risks.
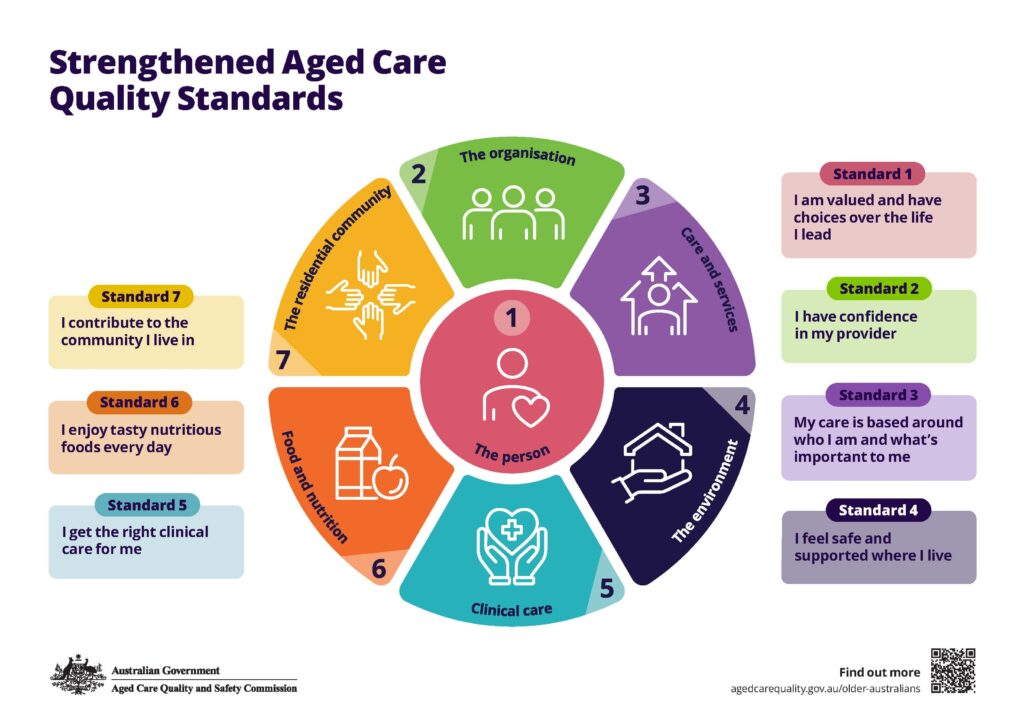
Strengthened Aged Care Quality Standards
The Aged Care Quality Standards have been strengthened under the new Aged Care Act and new regulatory model in response to the Aged Care Royal Commission, which found they did not adequately support:
- Food, nutrition, and the dining experience of older people in residential aged care
- Care of people living with dementia
- Care for people from diverse groups, notably, Aboriginal and Torres Strait Islander people.
- Effective and accountable governance
- Clinical care and the management of clinical risk
The old Aged Care Quality Standards, comprising eight standards, has been superseded by the Strengthened Aged Care Quality Standards, which combine some old standards and introduce new ones.
The diagram below provides a simple overview of the incoming new standards.
Note that providers of Support at Home, depending on their registration category, are required to meet Standards 1 through 5. Only Residential Care Providers are also required to meet Standards 6 and 7.
For Residential Care Providers, there is a significant strengthening of the regulation of food and nutrition to ensure that people living in residential care are provided with nutritious and tasty food, as well as an enjoyable dining experience, that meets their preferences and assessed needs, upholds their dignity, and delivers real choice.
New Regulatory Model and Registration Process
- All providers of aged care services need to be registered with the Commission.
- Approved providers, known as Registered Providers, and each provider must meet obligations based on the types of services they deliver. Those listed in the previous section are a minimum requirement for all providers.
- A risk-based approach to regulation, similar to that used for NDIS, is introduced, that is, the level of regulatory oversight is proportionate to the complexity of care provided.
- Universal provider registration is in place; that is, even providers who deliver multiple programs, such as home care and residential care, only needs to register once.
- Standard registration periods is 3 years; however, longer periods may be allocated to providers who consistently meet or exceed their obligations and quality of care, and shorter periods may apply to new providers or those with a record of non-compliance to ensure risk to individuals is managed appropriately.
- All existing aged care and CHSP providers are deemed across into registration categories appropriate to their care and services and their previous performance in delivering those care and services. For more information about the deeming process, go to this link: The deeming process – transitioning providers to the new system.
Registration of New Providers
- The following entities can now apply to be registered providers:
- Companies
- Cooperatives
- Government entities
- Incorporated entities
- Other unincorporated associations with a governing body
- Sole traders
- Partnerships
- The assessment of the suitability of new organisations or people to become registered aged care providers is similar to the old provider approval process, with some terminology changes and an audit process depending on the registration categories sought.
- Prospective providers are required to complete an application form, which is different to the one previously used. The application forms are available on the Aged Care Quality and Safety Commission website.
- Applicants are assessed for suitability, experience, performance and compliance in relation to the care they currently provide, and financial viability, as well as the responses in their application.
- General requirements include:
- An organisation or person must have an ABN
- Each Responsible Person must be suitable to deliver aged care services
- Must have a record of and systems for sound financial management
- Must meet all registration category-specific requirements
- Experience in delivering aged care or similar services, such as NDIS
- Demonstrated performance in delivering services relevant to aged care, for example, outcomes of NDIS audits
- Legal and business structure, including associated entities such as subcontractors and outsourced services
- Audits against the Quality Standards are then conducted as part of the registration process for registration in categories 4, 5, and 6 (explained in the next section), if the applicant is found to meet the general requirements described above. Conformance demonstrated during the audit assures the Commission that the prospective provider can deliver care and services that meet the Quality Standards and reduce risk to individuals. I
- Prospective providers wishing to become registered providers of residential aged care must seek approval for at least one residential care home through the Aged Care Quality and Safety Commission in a separate process to be eligible to apply for registration.
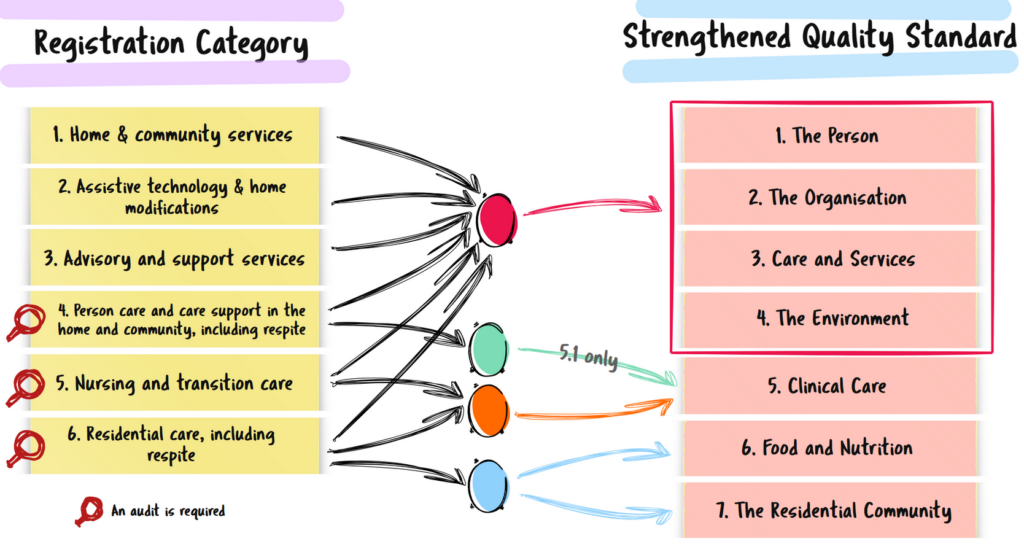
Registration Categories
Six registration categories follows a risk-based approach in grouping service types based on complexity and risk. Therefore, the registration requirements and associated provider obligations are risk-proportionate, as is the regulatory oversight applied. Providers registered into categories 1, 2 and/or 3 must meet standard provider obligations and must ensure they deliver care and services in accordance with the Strengthened Aged Care Quality Standards, but are not subjected to audits by the Aged Care Quality and Safety Commission.
Providers registered into categories 4, 5 and/or 6 must comply with the Strengthened Aged Care Quality Standards and are audited by the Commission.
The following table summarises the way the new regulatory model is applied based on registration categories:
| Reg Category | Description | Service Types | Provider Obligations | Code of Conduct | Audit of Standards |
|---|---|---|---|---|---|
| 1 | Home & community services |
|
YES | YES | NO |
| 2 | Assistive technology & home modifications |
|
YES | YES | NO |
| 3 | Advisory and support services |
|
YES | YES | NO |
| 4 | Person care and care support in the home and community, including respite |
|
YES | YES | YES
1, 2, 3, 4 + 5.1 (Clinical governance) |
| 5 | Nursing and transition care |
|
YES | YES | YES
1,2,3,4,5 |
| 6 | Residential care, including respite |
|
YES | YES | YES
1,2,3,4,5 + 6 & 7 |
Registration Categories Vs. Strengthened Quality Standards
Let’s clarify one of the most common sources of confusion: how, as a provider, your registration category relates to the Strengthened Aged Care Quality Standards, and whether or not you’ll be audited.
On the left-hand side of the following picture, you’ll see the six registration categories mentioned above.
You’ll also notice the arrows connecting each registration category to different areas of the Strengthened Quality Standards. These show which standards each provider must comply with. For example, if you are registering under categories 1, 2, and 3, your application must address Standards 1 through 4. If you are registering under category 4, in addition to standard 1 to 4, you should address standard 5.1, which is a proportion of standard 5.
If you provide registration category 5, you must meet Standards 1 to 5. And. In some cases, such as residential care, you need to meet all seven standards.
So, in summary, the registration category you select determines which quality standards apply to your service in addition to other requirements, such as the Code of Conduct and Provider Obligations that are applicable to all registration groups.
Now, look at the red magnifying glass icon. That means an audit is required for that registration category — so Categories 4, 5, and 6 are be audited as part of the registration process, but the registration Categories 1, 2, and 3 may be required to demonstrate compliance if their registration is ever at risk due to a serious complaint or other event.
Renewal of Registration
Registered providers are invited by the Commission to renew their registration prior to the expiry of their current registration period, and then the following steps will occur:
- Providers confirm their intention to renew their registration
- The Commission issues an audit invoice.
- For providers registered in categories 4, 5 and 6, the Commission then conducts a quality audit against the quality standards, which includes an assessment of the organisation’s governance systems, and the way care is delivered, including care experience and outcomes for individuals. The Commission has introduced a Care Delivery Evidence Collection Tool (CDECT).
- Providers apply to the Commission to renew their registration by completing an Application Form. Renewal of registration is then be based on:
- information set out in the renewal application form
- the quality standards audit
- routine provider reporting
- notifications
- information from complaints
- outcomes from any risk-based monitoring or compliance actions
Single Assessment
This new system provides a single assessment pathway for individuals, including when their needs change. The Single Assessment System workforce commenced operations at the end of 2024, amalgamating three different assessment workforces: the Regional Assessment Service (RAS), the Aged Care Assessment Teams (ACAT), and AN-ACC assessors for residential care. The assessment tool now used to determine eligibility for government-subsidised aged care is the Integrated Assessment Tool (IAT).
New First Nations assessment organisations were stood up from 1 November 2025 to ensure that culturally safe and appropriate pathways are available for Aboriginal and Torres Strait Islander people eligible for aged care services.
Statement of Rights
Under the new Aged Care Act 2024, the Charter of Aged Care Rights has been replaced with the Statement of Rights. The Statement of Rights is similar to the Charter, but the language has been strengthened to align with the rights-based new Aged Care Act, providing enhanced descriptions of each individual’s rights and clarity to aged care providers about their obligations and the consequences of breaching these rights.
A fact sheet about the Statement of Rights can be viewed at this link: A new Aged Care Act for the rights of older people
Application and Audit Fees
Under the new Aged Care Act, the charging arrangements is different.
There is new charging arrangements for assessing applications, as well as any audits they do for the applications, if applicable.
The tables in the link below outline the fees the government charges under the new Aged Care Act.
https://www.agedcarequality.gov.au/sites/default/files/media/fee_comparison_tables_august_2025.pdf
Key Features of the Support At Home Program
Strengthened Aged Care Quality Standards
Providers registered to deliver care and services under the new Support at Home Program are required to meet Strengthened Standards 1 to 4 and may need to meet some or all outcomes under Standard 5 if they deliver services from categories 4 and 5.
Providers registered in categories 1, 2 and/or 3 are not audited against the Strengthened Standards unless the Commission believes participants are at risk; however, providers registered in categories 4 and 5 are audited as part of the registration and renewal processes.
Existing and prospective home care providers should read this full blog to understand all the changes to aged care programs, the regulatory model, and the Strengthened Aged Care Quality Standards.
Program types
The Support at Home Program has encompassed the Home Care Package Program and the Short-term Restorative Care Program.
CHSP and other specialised programs will transition under the Support at Home Program no earlier than 1 November 2027.
Single provider model
Participants under the Support at Home Program have their services managed by a single provider, and it is a requirement that all participants receive care management.
This means that any registered provider wishing to receive the participant’s subsidy must be registered in Category 1 to 4 at least and provide personal care and care management. They are also required to meet Outcome 5.1 Clinical Governance under the Strengthened Quality Standards (see Registrations Categories).
To deliver and therefore claim for nursing services, registered providers also need to be registered in Category 5.
Classification and Funding Levels
There are eight classification levels (previously 4 levels under HCP), and the eighth funding level exceeds the HCP level 4 package by around $16,000 annually.
These are the indicative budget amounts for each classification level. Please note that these are subject to indexation revision.
| Class | Quarterly Budget | Annual Amount |
|---|---|---|
| 1 |
$2,683.01 |
$10,732.04 |
| 2 |
$4,008.91 |
$16,035.64 |
|
3 |
$5,491.67 |
$21,966.70 |
| 4 |
$7,424.07 |
$29,696.28 |
| 5 |
$9,924.40 |
$39,697.61 |
|
6 |
$12,028.44 |
$48,113.41 |
|
7 |
$14,536.88 |
$58,147.50 |
| 8 |
$19,526.51 |
$78,106.04 |
* Effective from 1 November 2025 and subject to change in March and September each year in line with indexation.
There are also additional funding streams for Assistive Technology and Home Modifications (AT-HM) that would previously have been deducted from the Home Care Package budget. These tiered funding amounts are allocated based on the assessed need of the participant, that is, low, medium or high. For example, a participant with complex needs would be allocated a high tier of funding to ensure all goods and equipment required for their care can be purchased.
Participants also have access to short-term funding supports such as the Restorative Care Pathway (replacing the Short-term Restorative Care Program) and the End-of-Life Pathway (new funding). Participants accessing these pathways can also access AT-HM funding to purchase goods, equipment, or home modifications to meet their needs.
The table below outlines the expected amounts for other funding streams.
| Assistive Technology | Home Modifications | Restorative Care Pathway | End of Life Pathway |
|---|---|---|---|
|
Low – $500 |
Low – $500 | $6000 | $25000 |
| Medium – $2,000 | Medium – $2,000 | Plus AT-HM funding |
Plus AT-HM funding |
|
High – $15,000 |
High – $15,000 | 16 Weeks | 12 Weeks |
| Must be spent within 12 months | Must be spent within 12 months.
Capped at $15K over lifetime. |
Restorative care management is undertaken by a clinically qualified Care Partner. |
Same services as under SAHP |
Overall, the higher classification levels (up to 8) and the additional funding streams described in the table above mean that participants of the Support at Home Program have access to high levels of funding to keep them at home for longer.
Care Domains
Under the Support at Home Program, service types are grouped into three care domains. These are also the basis of participant contribution levels, with service types supporting everyday living attracting the highest contribution level in recognition that these services – such as cleaning, home and garden maintenance, and delivery of meals – are not usually subsidised by the government at any other stage of life. The table below demonstrates this new approach:
| Category | Service Types | Participant Contribution Level* |
|---|---|---|
| Clinical Supports |
|
None – The government fully fund these services for all participants |
| Independence |
|
Moderate – Recognising that these services contribute to overall wellness, reduce hospitalisation and delay entry to residential care. The contribution rate range is expected to be between 5% and 50%. |
| Everyday Living |
|
High –The contribution rate is expected to be between 17.5% and 80% in recognition that the government does not usually subsidise these services at any other time in a person’s life. |
* Participant contribution levels are yet to be finalised.
Capped Pricing
Price caps on services under the Support at Home Program will be developed by the Independent Health and Aged Care Pricing Authority and will apply from 1 November 2026.
From 1 November 2025, and until capped pricing commences, providers are expected to set their own prices. For guidance on setting prices for the 2025 financial year, it is recommended that you consider the information contained in the Summary of Indicative Support at Home Prices Factsheet published by the Department of Health and Aged Care, which contains price ranges reflecting what the Home Care Package providers state they are intending to charge under Support at Home.
Summary of indicative Support at Home prices
Don’t forget – if you are an existing provider with home care package clients transitioning over to the Support at Home Program, you must discuss and agree on your intended price changes with your clients as soon as possible and provide them with a new service agreement. Information about transitioning existing home care package clients can be found in the Support at Home Program Manual and the Support at Home program provider transition guide.
CHSP will maintain current CHSP national unit price ranges with standard indexation applied annually, as usual. Price loading will now include MM5.
Care Management
- Care management is classified under the Clinical Supports care domain.
- Care management funding is now capped at 10% of the participant’s quarterly budget. This is deducted and kept in a pooled care management account held by Services Australia.
- Providers can use the funding in that account for any of their participants flexibly, accessing it through claiming for care management activities for ongoing services.
- Care management is undertaken by suitably qualified Care Partners who must deliver a care management activity at least monthly.
- Care Partners must hold clinical qualifications if they provide care management to clinically complex participants or participants receiving funding through the Restorative Care Pathway.
- Care Partners for participants receiving services through the Restorative Care Pathway must be AHPRA Registered Nurses or Allied Health Professionals.
Package Management
Package management is no longer a separate billable service type, and the costs that were previously covered by this fee under the Home Care Package Program are now expected to be incorporated into service pricing (see information under Capped pricing).
Supported Decision Making Framework
Supported decision-making involves helping an individual (previously referred to as consumer or older person), make or communicate their own decisions, thereby maintaining control over their lives.
A key feature of the new Act is the presumption that every individual has the ability to make decisions, and recognition that some may want or need support to make those decisions.
Under the new Act, individuals can choose who can support them in making decisions, when and if they want or need support, and these people are known as registered supporters.
Registered supporters can be individuals who also hold a guardianship or power of attorney role, or they can be trusted family members or friends. The difference is that a registered supporter who is not a guardian or power of attorney does not have decision-making power on behalf of the individual; their role is to support the individual to make their own decisions.
The registered support role replaces the roles of regular and authorised representatives in My Aged Care.
More details about this important change can be viewed here: Department of Health and Aged Care – Supported Decision Making.
New Financial and Prudential Standards
These new standards have been implemented to strengthen financial governance and thereby support and improve the sustainability of aged care providers, ensuring they can deliver high-quality care to individuals and minimise risk to care continuity. They replace the old four Prudential Standards (Governance, Liquidity, Disclosure, and Records), and from 1 November 2025, some home care providers have been required to meet them.
The changes are summarised as follows:
- The new Financial and Prudential Management Standard replaces the old Governance Standard.
- The Liquidity Standard remains but has been strengthened.
- The Investment Standard is new and ensures residential care providers manage and monitor investments responsibly, including those made with refundable accommodation deposits.
- The Disclosure and Records Standards are moved into the New Aged Care Act Rules, which have not yet been finalised.
| Old Standards | New Standards |
|---|---|
| New Standards | Financial and Prudential Management Standard |
| Liquidity Standard | Liquidity Standard (Strengthened) |
| Disclosure | Moved into the New Aged Care Act Rules |
| Records | Moved into the New Aged Care Act Rules |
| Investment Standard |
The new standards and the provider categories they apply to are as follows:
| Standards | Who it applies to |
|---|---|
| Financial and Prudential Management Standard | Category 4 & 5 Home care providers
Residential care providers* |
| Liquidity Standard | Residential care providers* |
| Investment Standard | Residential care providers* |
*Excluding government entities and local government authorities.
More information can be viewed here: The new Financial and Prudential Standards.
Aged Care Data and Digital Strategy 2024–2029
The Australian Government’s Aged Care Data and Digital Strategy 2024–2029, as a key component of the broader Aged Care Reform, outlines a transformative vision for aged care, emphasising person-centred services, streamlined operations, and enhanced digital capabilities. To thrive in this evolving landscape, aged care providers must adopt innovative solutions that align with these strategic priorities.
Key Strategic Priorities:
-
Enhancing Digital Maturity: Building and embedding data and digital maturity across the sector to support efficient, high-quality care.
-
Optimising Data Utilisation: Improving data collection and utilisation to inform better decision-making and service delivery.
-
Strengthening Care Connections: Integrating aged care support plans with My Health Record to ensure coordinated and continuous care.
-
Reducing Administrative Burden: Automating data sharing between providers and the government through initiatives like the Business to Government (B2G) developer portal.
What can Existing Registered Providers Expect?
Home Care Providers
- If they have not already contacted you, the Aged Care Quality and Safety Commission will commence communicating with you about deeming you into registration categories under the new Universal Registration model and ensuring that you then review their decision.
- You should immediately familiarise yourself with the Support at Home Program Manual and associated resources. See key resources at the Links to Key Resources.
- The difference between the Home Care Package Program and the Support at Home Program is significant; therefore, existing providers should plan their transition as soon as possible to ensure their organisation, workers, and clients are ready.
- There are numerous steps required for transition, and it would not be practical to attempt to summarise them in this blog. Instead, we recommend you access the Support at Home Provider Transition Guide at this link: Provider Transition Guide
- The Transition Guide provides detailed information about the steps providers should take and includes recommended timeframes for completion.
- Grandfathering arrangements apply to home care package recipients who, as of September 12, 2024, were either receiving a Home Care Package through the National Priority System or had been assessed as eligible for one. These arrangements ensure that grandfathered HCP recipients won’t face reduced support or higher costs under the new Support at Home contribution rules. Details on grandfathering arrangements are available in the Support at Home Program Manual.
Flexible Care Providers
- The Short-term Restorative Care Program ceased on 30 October 2025 and was replaced by the Restorative Care Pathway under the Support at Home Program.
- If they have not already contacted you, the Aged Care Quality and Safety Commission will commence communicating with you about deeming you into registration categories under the new Universal Registration model and ensuring that you then review their decision.
- You should immediately familiarise yourself with the Support at Home Program Manual and associated resources. See key resources at the Links to Key Resources.
- The way care and services are delivered through the Restorative Care Pathway under Support at Home Program is similar in many ways to the STRC Program in terms of multidisciplinary care and goal planning, however, the way in which it operates within the Support at Home Program, including how funding is claimed, is quite different; therefore, existing providers should plan their transition as soon as possible to ensure their organisation, workers, and clients are ready.
- We recommend you access the Support Home Provider Transition Guide at this link: Provider Transition Guide.
- Please note that the Commission and the Department of Health and Aged Care have not yet finalised some information about restorative care.
Residential Care Providers
Reforms impacting residential care are still being finalised and released; however, here are some changes existing providers can expect:
- Residential providers have commenced reporting on the total number of operational beds and 24/7 Registered Nurse coverage from November.
- Places are no longer allocated to residential care providers but are assigned directly to individuals who access government-funded residential care services; therefore, mainstream residential care providers no longer need an allocation of places to deliver government-funded aged care services. Providers who provide specialist aged care programs, such as Transition Care, still need to be allocated places. More information on the Places to People changes can be viewed here: Places to people – Embedding choice in residential aged care
- New Higher Everyday Living Fee (to be finalised)
- Changes to accommodation funding, including:
- An increase in the accommodation price cap from $550K to $750K
- Refundable Accommodation Deposit retention fees of 2% can be deducted monthly, capped for 5 years.
- Daily Accommodation Payment to be indexed twice a year.
CHSP Providers
From 1 November 2025, CHSP providers are subject to the new Aged Care Act 2024 and will be regulated in the same manner as other aged care programs.
CHSP providers will be required to register with the Aged Care Quality and Safety Commission and be deemed into applicable registration categories for each service delivered under the new universal provider registration. For example, a CHSP provider delivering Domestic Assistance and Home Garden Maintenance will be registered under Category 1. If the same provider provides personal care, they will be registered under Category 4. The Commonwealth Home Support Program will be known as a Specialist Aged Care Program.
CHSP providers must also comply with the new Aged Care Act, including meeting provider obligations relating to the following:
- The Code of Conduct for Aged Care
- Worker screening requirements
- Personal information and record keeping
- Fees and payments
- Incident management and reporting under the Serious Incident Response Scheme
- Continuity of Care (known as security of tenure)
- Service planning
- Complaints and whistleblowers
- Rights and Principles
- Compliance with laws and regulations
More details can be viewed at this link: The new regulatory model: Guidance for CHSP providers
CHSP providers will commence monthly reporting through the Department of Social Services’ Data Exchange, against the new Act-associated service list, which includes the client’s My Aged Care ID. From October 2025, more details are required in this reporting relating to travel, meals, settings, timing, etc. The Department will issue a provider toolkit and access to a staging environment (for testing changes and interfaces) to assist with these changes.
A fact sheet outlining the proposed changes to Data Exchange (DEX) reporting can be viewed here: Data Exchange from 1 July 2025 – Fact sheet
The way CHSP services are described, regulated and delivered will change to align with the Support at Home Program, and standardise the service list across all in-home aged care programs. This means that the names of many service types and services will change, and inclusions and exclusions will be defined and clarified for some services.
A fact sheet outlining the changes can be viewed at this link: Proposed changes to the CHSP Service List from 1 November 2025
If you have not yet seen all the changes coming to CHSP, it is recommended that you review this webinar on the Department of Health and Aged Care website:
Commonwealth Home Support Programme 2025-2027 extension and reforms update
CHSP will not transition to the Support at Home Program on 1 November 2025 with HCP and STRC providers, but it is expected to transition on or after 1 July 2027. In relation to that timeline, the 2025-2027 extension process is underway with a new grant agreement that will be valid for two years from 1 November 2025.
At this time, there are no changes to the current client contribution arrangements for CHSP.
How Can I Ensure I Deliver High-Quality Care to Individuals?
- Engage qualified, competent, suitable workers
- Stay up-to-date with regulatory changes
- Listen to your clients and workers
- Monitor risks, incidents, and complaints
- Undertake regular Self-assessments and internal audits
- Comply with and exceed the Aged Care Quality Standards
- Follow the quarterly Sector Performance Reports issued by the Commission, ACQSC Sector Performance.
How Can I Stay Up-to-Date?
- Tune into this blog
- Consider resources available through ISO Consulting Services, which consistently align with the most recent legislative changes and best practices.
- Stay connected with the resources listed in the Sections for links to key resources for the most current information
- Subscribe to updates from:
- Department of Health and Aged Care – Subscribe to aged care newsletters and mailing lists
- Aged Care Quality and Safety Commission – Subscribe to ACQSC bulletins
How Can I Prepare to Meet the Strengthened Aged Care Quality Standards?
Existing Providers
Existing providers should ensure they understand which Strengthened Aged Care Quality Standards apply to their registration categories and how they will be expected to demonstrate compliance.
If you are already delivering aged care under the Commonwealth Home Support Program, the Home Care Packages Program, or the Short-term Restorative Care Program, or you are a Residential Care provider, the key steps are:
- Ensure you understand the Strengthened Aged Care Quality Standards and how they differ from the old standards.
- Access the Strengthened Quality Standards Provider Guidance to assist your preparation, to understand what quality care looks like to individuals receiving it, and to comply with quality audits when they occur: Strengthened Quality Standards – Provider Guidance
- Educate your workers as soon as possible about the new standards.
- Undertake a self-assessment against the new standards (you can contact us to enquire about the FREE Gap Assessment Tool, offered as part of ISO+™ — an all-in-one Aged Care compliance and operations software)
- Develop and implement corrective actions to resolve any gaps identified in the above self-assessment.
- Review and update all your policies and procedures to ensure they meet or exceed the new standards.
- Review all your existing processes and systems to ensure they will continue to support your compliance with the new standards.
We recommend that you use the following checklist to prepare your organisation and your workers to meet the Strengthened Aged Care Quality Standards: Provider Readiness Checklist.
The Commission has also released Draft Audit Evidence Collection Tools (AECT) that are intended to be used as part of the audit process for existing providers who are renewing their registration or who wish to vary their registration. Two evidence collection tools are used for existing providers, one focusing on systems and processes, and the other is used to collect evidence associated with care being delivered to participants, to ensure those systems and processes are being applied to care delivery and that care is safe, high-quality, and meets the expectations of participants. As recommended for new providers, existing providers would also benefit from downloading these tools and undertaking audit preparation activities to ensure their processes are compliant with the new Aged Care Act, the Strengthened Aged Care Quality Standards, and the Support at Home Program (for home care providers).
- Draft Audit Evidence Collection Tool – Registration Renewal
- Draft Audit Evidence Collection Tool – Registration Variation
- Draft Care Delivery Evidence Collection Tool – Home Care Providers
- Draft Care Delivery Evidence Collection Tool – Residential Care
New Providers
New providers should also ensure they understand which Strengthened Aged Care Quality Standards apply to their registration categories and how they will be expected to demonstrate compliance.
As you register as a new aged care provider after 1 November 2025, the Commission will audit you against the Strengthened Standards as part of your registration process and conditions if you are seeking registration in categories 4, 5, or 6; therefore, you must be able to demonstrate compliance prior to commencing care delivery. If you are seeking registration in categories 1, 2, or 3, although you will not be audited, you must still deliver care and services in accordance with the Strengthened Aged Care Quality Standards, and you would be expected to demonstrate this if requested by the Commission.
We recommend taking the following steps prior to submitting your application for registration:
- Ensure you understand the Strengthened Aged Care Quality Standards.
- Access the Strengthened Quality Standards Provider Guidance to assist your preparation, to understand what quality care looks like to individuals receiving it, and to prepare evidence in readiness for your quality audit: Strengthened Quality Standards – Provider Guidance
- Educate your workers as soon as possible about the new standards.
- Undertake a self-assessment against the new standards (you can contact us to enquire about the FREE Gap Assessment Tool, offered as part of ISO+™ — an all-in-one Aged Care compliance and operations software)
- Develop and implement corrective actions to resolve any gaps identified in the above self-assessment.
- Develop all your policies and procedures to ensure they meet or exceed the new standards.
- Develop or select processes and systems that support compliance with the new standards.
We recommend that you use the following checklist to prepare your organisation and your workers to meet the Strengthened Aged Care Quality Standards: Provider Readiness Checklist.
The Commission has released a Draft Audit Evidence Collection Tool (AECT) that it intends to use as part of the audit process for the registration of new providers. Please remember this is a draft document and may change before 1 November.
Links to Key Resources
Department of Health and Aged Care
- New Aged Care Act Webpage
- New Aged Care Act – Sector Change Plan
- The deeming process – transitioning providers to the new system
- Quality obligations for providers
- Department of Health and Aged Care – Residential Aged Care Provider webpage
Support At Home Program
- Department of Health and Aged Care – Support at Home webpage
- Support at Home Program Manual
- Support at Home Program Handbook
- Support at Home Program Provider Transition Guide
- Support at Home – Claims and Payments Business Rules Guidance
Commonwealth Home Support Program
Aged Care Quality and Safety Commission Resources
- Reform Changes for Providers
- Provider Registration Policy
- Sector Readiness Plan
- Commission Sector Webinars
Strengthened Aged Care Quality Standards
- ACSC Strengthened Quality Standards
- Strengthened Aged Care Quality Standards – provider training presentation
- Provider Registration Policy
- Strengthened Quality Standards – Provider Guidance
Financial and Prudential Standards
Our expertise is to help our clients develop, implement, certify and maintain their management system through a hassle-free process and with a…
Read MoreThe National Disability Insurance Scheme (NDIS) provides about 460,000 Australians under the age of 65 with a permanent and significant disability with…
Read MoreAs the aged population is growing in Australia, the need for a range of care, accommodation, hospitality, and other services is undeniable. To address this growth…
Read More