The Australian Government is determined to deliver reforms to Australia’s aged care system that improve the care provided to older Australians and has implemented the first two years of an $18.8 billion five-year Aged Care Reform program from 2021 to 2024 (postponed to 2025) in response to the Royal Commission into Aged Care Quality and Safety Final Report: Care, Dignity and Respect (Royal Commission).
The aged care reforms will put older Australians first, improving quality, safety, and choice in Aged Care to create a sector that:
- is responsive to the needs of older Australians
- is simpler to navigate, with face-to-face services
- empowers older Australians to make informed choices
- is well regulated
- is more transparent
- makes sure providers are accountable
- values and grows the aged care workforce.
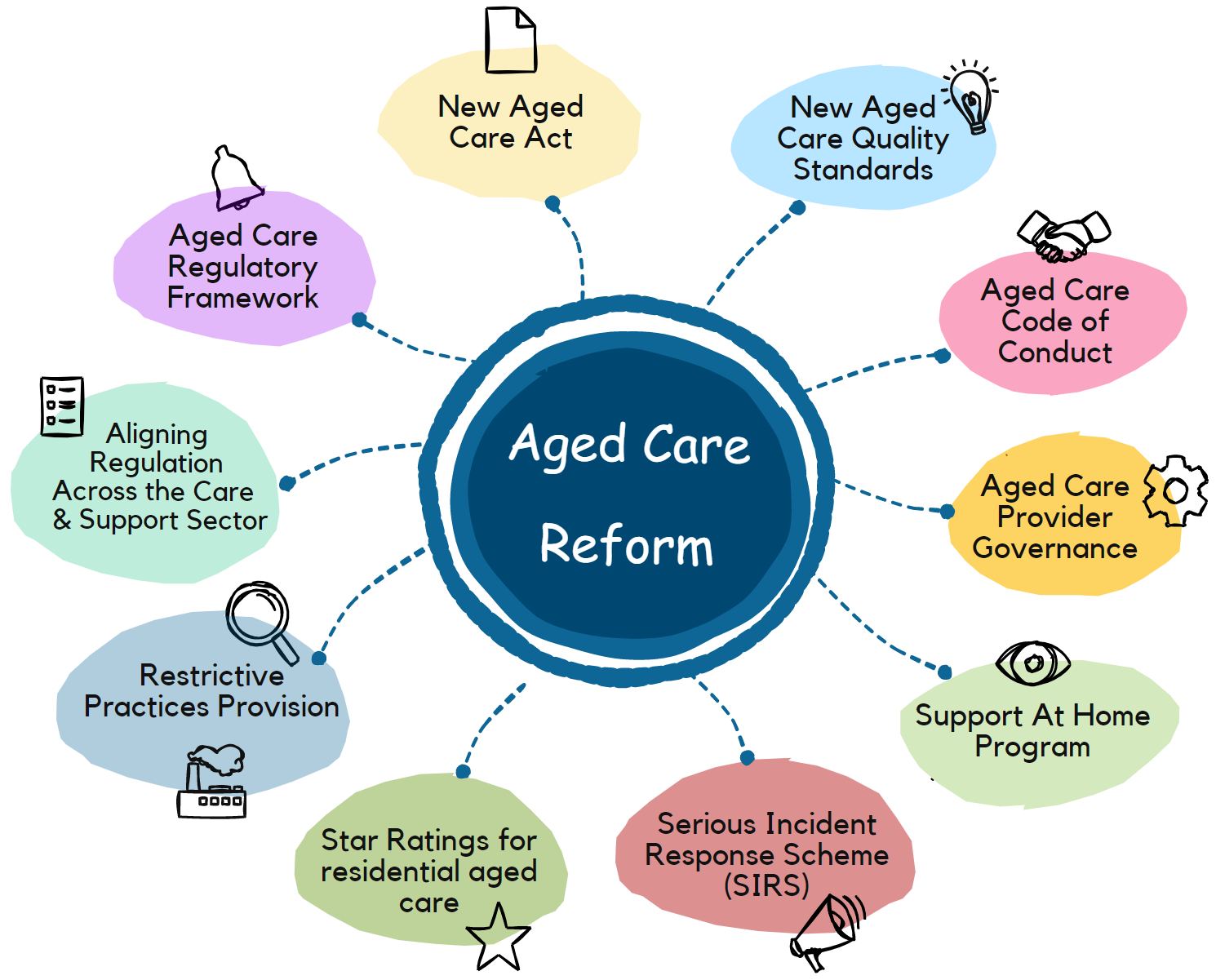
This reform has already started with some changes, such as the Code of Conduct for Aged Care, Serious Incident Response Scheme (SIRS), etc. It will continue with other changes that will be introduced by July 2025. In more detail, we have summarised some of the most significant changes relevant to the providers below. As the changes will be made gradually, this blog will be updated accordingly to the best of our knowledge.
Aged Care Regulatory Framework
More than 50 of the 148 recommendations of the Royal Commission require the introduction of supporting legislation. The new Act will put older Australians and their needs at the centre of the legislative framework and underpin generational reform of aged care in Australia. The Royal Commission also highlighted that the current regulatory framework is no longer suitable. Current regulatory framework constraints include, but are not limited to:
- One-size-fits-all providers: for example, the same obligations apply to home care regardless of the services they provide; however, gardening service has different risks compared to a clinical care service regarding the risk of harm to the older Australian
- Only Corporations or state or territory governments can be approved aged care providers, but other types of businesses such as sole traders, partnerships, etc. Opening the market to other suitable providers will offer more choices to Older Australian.
- Current providers’ assessment is delivered through a pass/fail status, but not a graded assessment which does not provide the incentive to strive beyond a pass or fail and strive for excellence o innovation
- The current scheme does not allow legislative alignment or harmonisation between other care and support sectors, such as NDIS, considering that 60% of the providers do both Aged Care and NDIS.
The new regulatory model has four foundations:
- Rights-based approach – ensuring protections are in place to uphold the rights of older Australians.
- Person-centred approach – the needs, goals, values, and preferences of older Australians are at the heart of the regulatory model.
- Risk-based approach – strengthening the regulatory response through an aged care regulatory model based on risk.
- Continuous improvement approach – an ongoing commitment to enhancing the capability and quality of the aged care sector.
The design of the new regulatory model is being undertaken concurrently and collaboratively with related activities and reforms in the aged care sector, such as the new Aged Care Act, Reforming in-home aged care, and aligning regulation across the care and support sectors, such as aged care, disability support, and veterans’ care sectors.
New Aged Care Act
In response to the Aged Care Royal Commission, the Australian Government will invest $26.7 million to develop and introduce a new Act to underpin the fundamental and generational reform across aged care.
It includes the rights and principles and addresses significant structural changes within the Aged Care system. It also resolves many technical issues and ambiguities, such as the different definitions of a staff member and worker as an example. When writing this blog, the Aged Care and Other Legislation Amendment (Royal Commission Response) Act 2022 (No. 34, 2022) is in force. As an amendment of the Aged Care Act 1997.
The new Aged Care Act will replace the Aged Care Act 1997 and the Aged Care Quality and Safety Commission Act 2018. At the moment.
The new Aged Care Act establishes new requirements for aged care providers through 9 measures that respond to the Royal Commission into Aged Care Quality and Safety. Four of these measures directly relate to the regulation of Aged Care:
- Expanding the Serious Incident Response Scheme (SIRS) into home services
- Introducing a Code of Conduct for aged care providers, workers and governing persons
- Strengthening provider governance
- Ensuring consent to the use of restrictive practices.
SIRS in Home Care and Flexible Care
The Serious Incident Response Scheme (SIRS) is already in place for residential care services and settings, but from 1 December 2022, It also applies to home care and flexible care, including short-term restorative care in a home care setting, multi-purpose services and transition care, as well as the Commonwealth Home Support Programme (CHSP) provider.
They should review their Incident Management System (IMS) to ensure that it will continue to support them in improving the management and prevention of incidents.
They must also notify the Aged Care Quality and Safety Commission when reportable incidents occur as part of the Serious Incident Response Scheme (SIRS). Notifications must be made using the SIRS tile on the My Aged Care Service Provider Portal.
Code of Conduct for Aged Care 2022
It applies from 1 December 2022 to approved providers of residential, home, and flexible care, including short-term restorative care, multi-purpose services, and transition care. The Code of Conduct does not apply to the Commonwealth Home Support Programme (CHSP) and National Aboriginal and Torres Strait Islander Flexible Aged Care Program (NATSIFACP) as they are not approved providers under the Aged Care Act; however, these providers are still required to provide safe and respectful care and behave in a way that aligns with the Code. It is expected that similar provisions will be extended to all Commonwealth-funded aged care services as part of the planned introduction of a new aged care Act.
The Code includes eight elements that require the providers to:
- Respect people’s rights to express themselves and make decisions
- Treat people with dignity and respect and value their diversity
- Respect people’s privacy
- Provide high quality care in a safe and competent manner
- Act with integrity, honesty, and transparency
- Take action on quality and safety by promptly responding to issues and concerns
- Provide safe care free from all forms of violence and abuse
- Take reasonable steps to prevent and respond to all forms of violence, abuse and neglect, including sexual misconduct.
The Code is also consistent with the NDIS Code of Conduct with a focus on the individual’s right to receive quality care, but the Aged Care Code of Conduct has additional requirements, and the Aged Care providers must take reasonable steps to make sure workers (including employees, volunteers, and contractors)and governing people understand and comply with the Code.
The Commission has access to various compliance and enforcement actions to respond to different situations. In severe cases, actions may include banning a current or former worker or governing person from working in the aged care sector or, in the case of approved providers, applying a sanction or revoking their approved provider status.
Aged Care Provider Governance Reform
The Government’s Aged Care and Other Legislation Amendment (Royal Commission Response) Act 2022 implements nine measures to improve accountability and transparency and responds to 17 recommendations of the Royal Commission into Aged Care Quality and Safety.
From 1 December 2022, there are new governance responsibilities for all approved providers. Additional responsibilities will commence on 1 December 2023 for providers approved before 1 December 2022. They apply to approved residential, home and flexible care providers, including short-term restorative care, multi-purpose services and transition care, but Commonwealth Home Support Programme (CHSP) and National Aboriginal and Torres Strait Islander Flexible Aged Care Program (NATSIFACP). This does not apply to state/territory or local government authorities (which may be some MPS services).
These new requirements include:
- assess the suitability of their key personnel at least once a year
- submit material changes, including key personnel notifications, within 14 days regarding the suitability changes, employ new key personnel or leave a key personnel
- report annually on their operations.
- Set up a Governing Body including independent non-executive members with a mix of skills and experience, including at least one member with clinical care experience. This is not applicable to governing bodies with fewer than five members and provideside aged care to less than 40 care recipients, State or Territory body, State or Territory authority, local government authority, and Aboriginal Community Controlled Organisation (ACCO.
- Set up a quality care advisory body to support and inform the governing body
- Offer to establish at least one consumer advisory body to provide valuable feedback to the governing body
- The governing body ensures staff members have the appropriate skills, qualifications and experience necessary to fulfil their duties.
- Set up a constitution, including a set of rules controlling the operations of an organisation. This applies to the providers that are wholly owned subsidiaries
- report annually on their operations to the department
Restrictive Practices Consent Provision
Additional legislative amendments were made through the Aged Care and Other Legislation Amendment (Royal Commission Response) Act 2022. These further strengthened consent requirements to address gaps in state and territory legislation on the use of restrictive practices in residential aged care.
The Quality of Care Principles has been amended to include a hierarchy of persons/bodies who can consent to the use of restrictive practices on the care recipient’s behalf. This can only be used when:
- they cannot consent themselves
- there is no explicit legal avenue under relevant state or territory laws
- no one is appointed as the RPSDM due to delayed applications.
The hierarchy will only be in place until 1 December 2024. A new mechanism will be included in the new Aged Care Act.
This will ensure restrictive practices are only used with the appropriate consent to protect the health, rights and dignity of older Australians in residential aged care.
Revised Aged Care Quality Standards & Registration Process
In March 2021, the Australian Government announced an urgent review of Quality Standards. This was in response to the Royal Commission into Aged Care Quality and Safety Final Report: Care, Dignity and Respect (Royal Commission).
The Aged Care Quality standards are revised to make them:
- Person-centred – Care and services oriented around the individual
- Inclusive – Focused on governance, diversity, dementia, food and clinical care
- Measurable – Clear and easily implemented expectations
- Relevant – Applied based on service delivery types
- Coordinated – Aligns with the National Disability Insurance Scheme (NDIS)
In the revised standards, There are more details on what older people expect from their providers. It provides clear and details actions (142 actions) to help providers understand the requirements to achieve the desired outcome.
The requirements are more measurable and less subjective for a better assessment by the Aged Care Commission.
A new term, “older person/older people” will be used instead of the term “Consumer(s)” that is used in the current standards.
The term “Consumer” in the current standard
The following table summarises the differences between the current and revised standards drafted for public consultation:
| Current Standards | Revised Standards (Draft) | The Outcome of the Revised Standards |
|---|---|---|
| Standard 1: Consumer dignity and choice | Standard 1: The Person – I am valued and have choice over the life I lead
The revised Standard 1 is almost similar to the current Standard 1 |
|
| Standard 2: Ongoing assessment and planning with consumers | Standard 2: The Organisation – I have confidence in my service provider
The revised Standard 2 draws on the current Standards 6, 7 and 8 |
|
| Standard 3: Personal care and clinical care | Standard 3: The Care and Services – My care is based around who I am and what is important to me
The revised Standard 3 draws on Standard 2 and parts of Standards 3 and 4 |
|
| Standard 4: Services and supports for daily living | Standard 4: The Environment – I feel safe and supported where I live
The revised Standard 4 draws on Standard 5 and parts of Standard 3 |
|
| Standard 5: Organisation’s service environment | Standard 5: Clinical Care – I get the right clinical care for me
The revised Standard 5 draws on parts of Standards 2, 3 and 8 |
|
| Standard 6: Feedback and complaints | Standard 6: Food and Nutrition – I enjoy tasty and nutritious food every day
The revised Standard 6 expands significantly on parts of Standards 2 and 4 |
|
| Standard 7: Human resources | Standard 7: The residential Community – I contribute to the community I live in
The revised Standard 5 draws on parts of Standards 3 and 4 |
|
| Standard 8: Organisational governance | The revised Aged Care Quality Standard does not include Standard 8 | Not Applicable |
Current Aged Care Quality Standards apply to all providers regardless of the risk profile of the provider or the service type. It could lead to the over-regulation of some providers and the under-regulation of others. The new system has taken the modular concept of NDIS into consideration and is structured based on the type of services delivered by the providers. According to the revised standards, the Registration Categories and Registration Obligations for providers are summarised in the table below:
| Registration Category & Service Types | Registration Obligations | Registration Process and Period |
|---|---|---|
Category 1: Home and community services
|
|
|
Category 2: Assistive technology and home modifications
|
|
|
Category 3: Social support
|
|
|
Category 4: Clinical and specialised supports
|
|
|
Category 5: Home or community-based respite
|
|
|
Category 6: Residential care
|
|
|
Currently, the Commission is conducting a pilot to test the assessment process in 2023.
In Home Aged Care Reform and Support At Home Program
In-home aged care services such as the Home Care Packages (HCP) and Commonwealth Home Support Programme (CHSP) Program support almost one million senior Australians. Research shows that senior Australians want to remain at home for as long as possible before entering a residential aged care facility. More than 1 million Australian rely on aged care in their home today. With more than $9.5 billion in funding this financial year (FY 2022-23) going toward the in-home care program. Additional $40000 home care packages will be available this financial year.
In-home aged care reform seems to be needed:
- To improve access to services, reduce waiting time,
- To better align services to needs through the aged care assessments and manage unspent funds across CHSP and Home Care packages (HCP) are used for the people who are waiting for access to the funding and services
- To reduce unnecessary administrative costs and make sure the finding is going to care
- To better support independence at home. For example, more focus on preventative support that people might need, such as goods and equipment and home modification
- To make aged care simpler with better information and more transparency
The support At Home program that was introduced in January 2022 will replace Commonwealth Home Support Programme (CHSP), Home Care Packages (HCP) Program, Short Term Restorative Care (STRC) Programme, and Residential Respite. This model can be summarised in the followings:
- A new assessment and classification system is used and at the end of the assessment, Older Australian would agree on a support plan with their assessor that specifies units of individual services per month. For example, a support plan for 8 hours of personal care, 2 hours of domestic assistance, etc.
- Older Australians can choose one or multiple providers to deliver their services
- Providers would then be paid in arrears based on the services they have delivered at a subsidy rate set by the Government
- It uses use a Service List drafted in seven main categories as Independence at Home, Social Connections, Personal Care, Health and Specialised Support, Care Management, Digital technologies, equipment, home modifications, and Respite Care.
- There are also grants to support providers operating in thin market (narrow market)
- Goods, equipment and assistive technology (GEAT) and home modifications through a separate scheme to provide people with fast access to these services.
- There would be flexibility for providers to allow temporary or minor increases in services for clients without the need for reassessment
- If the client’s needs change significantly, at that point, they would be reassessed
- A Point of Delivery Payment Platform is being developed to enable providers to receive payments in real-time from both government and senior Australians
This new program is structured as:
- Short Trem Support for Independence
- Goods, Equipment, and Assistive Technology (GEAT) and Home modifications that are separately funded from the HCP budget
- Short Term allied health (similar to existing STRC program)
- Specialised support services, such as dementia, vision, or continence advisory services, that are grant-funded similar to the existing CHSP program)
- Ongoing Support At Home with a mixed funding model
- Activity-based funding based on a service list including the prices
- Supplementary grants for transport, cottage, and centre-based respite, meal, and social support groups as well as the providers who operate in thin or niche markets such as operating in a remote area or an urban setting
- Funding pool for additional client services (set as 25% of client budget each quarter)
- Client contributions and aligning what exists in HCP and CHSP
As the next step, after further consultations, It is expected to release the Government decision about this program sometime in Mid-2023 that give a 12-month for transition and implementation by July 2025.
In the meantime, the current CHSP and HCP are still available. No one will lose any in-home aged care services they currently have in place through the Commonwealth Home Support Programme or Home Care Packages Program.
Other Changes and Programmes of the Aged Care Reform
There are some other changes and new programmes running in parallel with the ones mentioned above, such as
- Residential aged care providers’ star rating system that is available directly to the public on My Aged Care from the late end of December 2022 to help older Australians and their families to compare the quality and safety performance of different services based on an overall Quality Rating and four sub-categories: Quality Measures, Compliance, Residents’ experience and Staffing minutes
- The new Aged Care Subsidy Calculation for Residential Care, known as AN-ACC (Australian National Aged Care Classification), as a replacement for ACFI from 1 October 2022 that responds to a key recommendation from the Royal Commission into Aged Care Quality and Safety. AN-ACC provides funding to approved aged care providers based on the type of service, and each resident’s care needs through three components: Base Care Tariff subsidy, AN-ACC classification subsidy, and initial entry adjustment payment for transitioning a permanent resident into a service.
The Aged Care reform will be continued with other changes, such as having nurses on-site 24/7 in Residential Care. Power of setting a cap on the administration and management fee for Home Care providers and mandatory reporting requirements, including financial information.
What ISO Consulting Services can do for you
As a prominent Aged Care and NDIS Registration consultant who has been assisting more than 1000 providers with the registration process, we are delighted to help you as well. If you’re interested in learning more about how ISO Consulting Services can assist with the Aged Care registration process and receive our Aged Care Registration packages that are developed in compliance with the most updated legislation and changes of the Aged Care Reforms, simply complete our Aged Care Questionnaire today. Alternatively, you can get in contact to discuss your options further with someone from our team.
Our expertise is to help our clients develop, implement, certify and maintain their management system through a hassle-free process and with a…
Read MoreThe National Disability Insurance Scheme (NDIS) provides about 460,000 Australians under the age of 65 with a permanent and significant disability with…
Read MoreAs the aged population is growing in Australia, the need for a range of care, accommodation, hospitality, and other services is undeniable. To address this growth…
Read More